What is SIADH?
The syndrome of inappropriate antidiuretic hormone secretion (SIADH) involves the excessive secretion of antidiuretic hormone (ADH) from the posterior pituitary gland or another source. ADH controls water reabsorption by the kidneys nephrons, causing the retention of water but not solute. Therefore ADH causes dilution of the blood which decreases the concentration of solutes such as sodium.
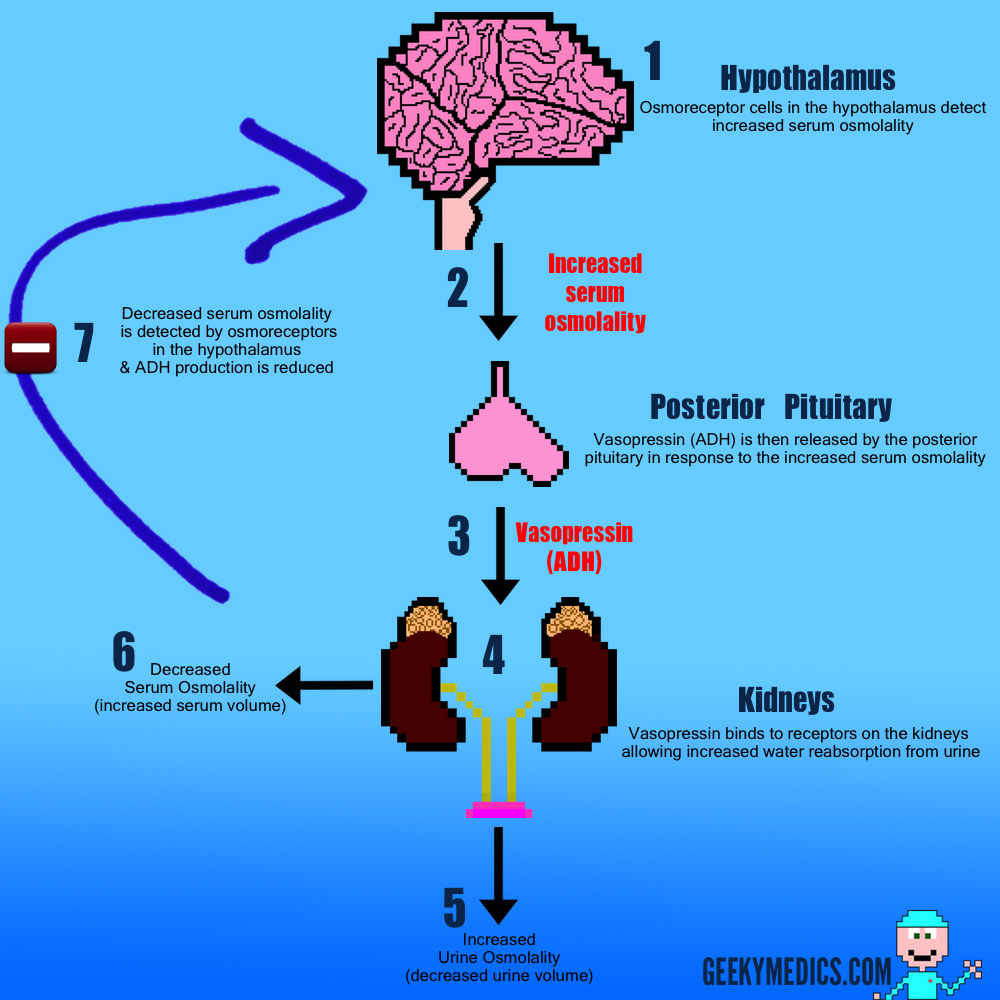
Physiology
Normal
1. Vasopressin (Anti-Diuretic Hormone) is produced by the hypothalamus in response to increased serum osmolality.
2. Vasopressin is then transported to the posterior pituitary gland.
3. It is then released into the circulatory system via the posterior pituitary gland.
4. It then travels to the kidneys where it binds to vasopressin receptors on the distal convoluted tubules.
5. This causes Aquaporin-2 channels to move from the cytoplasm into the apical membrane of the tubules:
- These aquaporin-2 channels allow water to be reabsorbed out of the collecting ducts and back into the bloodstream.
- This results in both a decrease in volume and an increase in osmolality (concentration) of the urine being excreted.
6. The extra water that has been reabsorbed re-enters the circulatory system, reducing the serum osmolality.
7. This reduction in serum osmolality is detected by the hypothalamus and results in decreased production of vasopressin.
Deranged physiology in SIADH
SIADH has a number of potential causes. These are demonstrated in the diagram below. The important difference in SIADH, is the lack of any negative feedback mechanism, resulting in an inability to reduce or stop ADH production. As a result, ADH is continually produced, regardless of what the serum osmolality is. This ultimately results in abnormally low levels of serum sodium and relatively high levels of urinary sodium, giving rise to the characteristic symptoms and signs associated with SIADH.

.
What causes SIADH?
Brain damage – Meningitis / Subarachnoid haemorrhage (SAH)
Malignancy – Small-cell lung cancer
Drugs – Carbamazepine / SSRIs / Amitriptyline
Infectious – Atypical pneumonia / Lung abscess /Cerebral abscess
Hypothyroidism
Signs and Symptoms
Symptoms¹
Symptoms vary greatly depending on the timescale of the development of hyponatraemia
Therefore mild hyponatraemia may cause significant symptoms if the drop in sodium is acute whereas chronically hyponatraemic patients may have very low serum sodium concentrations and yet be completely asymptomatic. This is thought to be due to cerebral adaptation, where brain cells can adapt their metabolism to cope with abnormal sodium levels, but this can only occur if the change in sodium concentration is gradual.
Mild – Nausea / Vomiting / Headache / Anorexia / Lethargy
Moderate – Muscle cramps / Weakness / Confusion / Ataxia
Severe – Drowsiness / Seizures / Coma
Signs¹
These also vary a great deal depending on the rate of serum sodium concentration change
- Decreased level of consciousness
- Cognitive impairment (short term memory loss / disorientation / confusion)
- Focal or generalised seizures
- Brain stem herniation – severe acute hyponatraemia (coma / respiratory arrest)
- Hypervolaemia –pulmonary oedema / peripheral oedema / raised JVP / ascites
Investigations³
Fluid status:
- Is the patient clinically or biochemically dehydrated?
- In SIADH this is not the case – the patient is either euvolemic or hypervolaemic
- If dehydration is present, it suggests another cause for hyponatraemia – diuretics / renal failure
Serum sodium – low in SIADH – <135 mmol/L
Serum potassium – if raised in the presence of hyponatraemia consider Addison’s
Plasma osmolality – this will also be reduced due to the low sodium concentration
Urine osmolality:
- Normally if serum osmolality is low, urine osmolality should also be low
- This is because the kidneys should be trying to retain solute
- In SIADH the excess ADH causes water retention but not solute retention
- As a result concentrated urine relatively high in sodium is produced, despite low serum sodium
Urine sodium :
- This will be relatively raised, in the context of the serum sodium concentration
TFTs – hypothyroidism is a cause of SIADH – ↓ T3 & ↑TSH would suggest this diagnosis
Serum cortisol – Addison’s causes ↓ Na, a low serum cortisol would suggest this diagnosis
Imaging – useful in detecting causes of SIADH such as small cell lung Ca
Diagnosis
The following features need to be present for a diagnosis of SIADH:³
- Hyponatraemia
- Low plasma osmolality
- Inappropriately elevated urine osmolality (>plasma osmolality)
- Urine [Na+] >40 mmol/L with normal salt intake
- Euvolaemia
- Normal thyroid and adrenal function
Management
It’s difficult to give a generic step by step management strategy for SIADH, as it can be due to so many different causes. As a result, you need to target your management strategy at the underlying cause for long term correction of sodium metabolism. Specialist endocrine input should be sought before commencing any of these management strategies.
Fluid restriction
This is a common management strategy for increasing serum sodium concentrations, at least temporarily, whilst the underlying cause is sought and treated. Usually the fluid restriction is between 1-1.5 litres per day. It’s largely dependent on patients co-operating with the treatment plan, which some patients can struggle with.
Replacing sodium
Another general management strategy for treating hyponatraemia is to replace sodium either orally or via IV fluid. This has to be done with great care, as if the sodium concentration is corrected too rapidly it can result in the devastating complication known as central pontine myelinolysis. This is characterised by permanent damage to the myelin sheath in the brain stem, causing acute paralysis, dysphagia, dysarthria, diplopia and decreased level of consciousness. As a result, this treatment strategy has to be carried out with extreme caution, with the recommendation of not correcting serum sodium levels more than 10 mmol/L/24h.
Examples of treating the underlying cause
Pneumonia – antibiotics
Carbamazepine – consider switch to alternative anti-epileptic i.e. sodium valproate
Hypothyroidism – levothyroxine replacement
References
Click to show1. Craig S; Hyponatremia in Emergency Medicine, Medscape, Apr 2010 (Symptoms & Signs)
2. Oxford handbook of clinical medicine 7th edition [p666-667]
3. Robert D. Zenenberg,Do, et. al (2010-04-27). “Hyponatremia: Evaluation and Management”. Hospital Practice. 38 (1): 89–96
The post Syndrome of inappropriate antidiuretic hormone secretion (SIADH) appeared first on Geeky Medics.